
The origin of highly mutated SARS-CoV-2 variants, including Omicron, is significantly attributed to prolonged infections in immunocompromised individuals, such as those with advanced human immunodeficiency virus (HIV) infection or cancer, where the virus can undergo extensive intra-host evolution [1] [2] [3]. In these individuals, a weakened immune system allows the virus to replicate for extended periods, providing ample opportunity for mutations to accumulate and for new variants to emerge under reduced immune pressure [1] [2] [4].
This phenomenon has been observed with several key variants:
- Omicron Variant: The Omicron (B.1.1.529) variant, which rapidly spread globally, was first isolated from an HIV-infected patient in Botswana, South Africa, in November 2021 [2]. Whole genome sequencing of Omicron revealed a multitude of mutations, with BA.1 containing 60 mutations compared to the original SARS-CoV-2, including 32 in the spike protein [2]. The high prevalence of HIV infection in South Africa is hypothesized to have contributed to the emergence of such highly mutated variants, as a large pool of immunocompromised individuals provides an environment conducive to prolonged viral persistence and evolution [2].
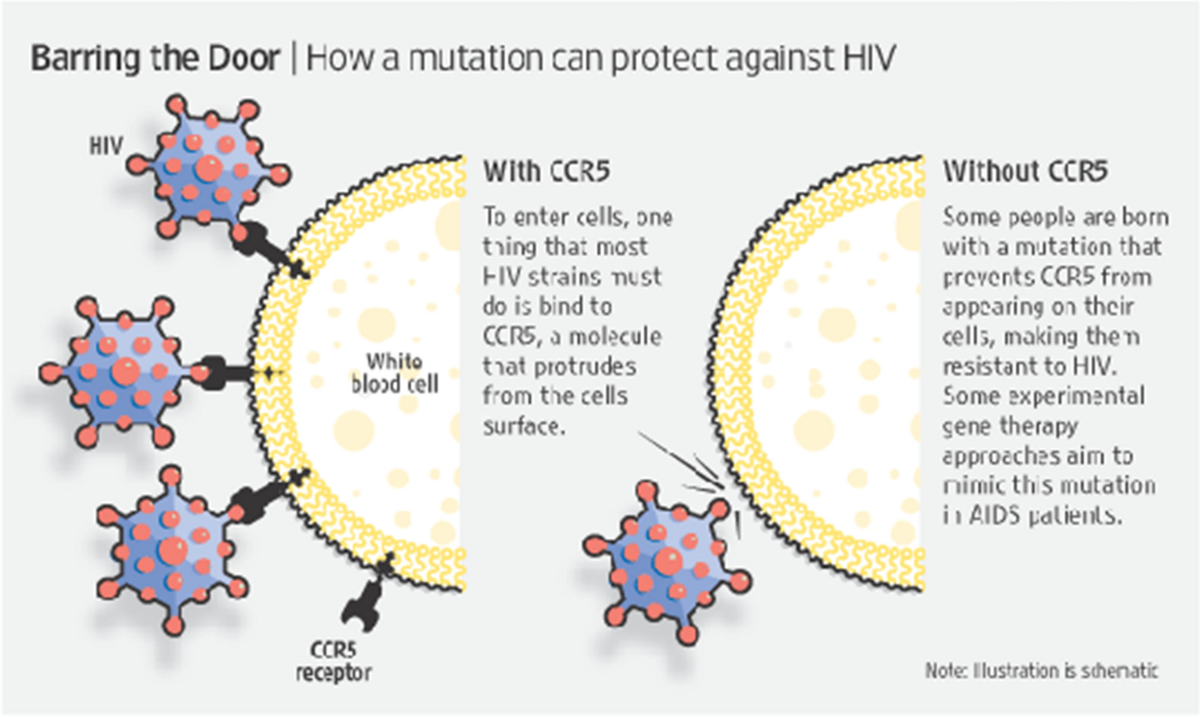
- Delta Variant Evolution: A case study described a patient with advanced AIDS who had a persistent SARS-CoV-2 Delta variant infection for over 80 days [1]. This Delta variant contained mutations (e.g., E484K, V3G) that were not commonly found in other circulating Delta viruses at the time, indicating significant intra-host evolution within the patient [1]. The patient's extremely low CD4+ T-cell count (2 cells/µL) and high HIV viral load contributed to their inability to clear the infection and mount an effective immune response [1].
- Alpha Variant: Similarly, the Alpha variant (B.1.1.7) was initially isolated from a cancer patient in the UK, suggesting that other forms of immunocompromised states can also predispose to the selection of novel coronavirus mutants [2].
In immunocompromised hosts, particularly those with advanced HIV disease, the immune system's inability to effectively clear the virus leads to sustained viral replication [1] [2]. This prolonged replication increases the chances of random mutations occurring, and those mutations that confer a selective advantage, such as improved transmissibility or immune escape, are more likely to be selected and propagated within the host [1] [4]. Studies have shown that people living with HIV (PLWH), especially those with low CD4+ T-cell counts and uncontrolled HIV viral loads, experience significantly longer durations of SARS-CoV-2 shedding compared to immunocompetent individuals [1]. For instance, a cohort study in South Africa found that PLWH with CD4 counts <200 cells/µL had a median shedding duration of 27 days, compared to 7 days in those with CD4 counts >200 cells/µL [1].
The implications of this phenomenon are significant for public health. It underscores the importance of ensuring access to effective antiretroviral therapy (ART) for PLWH, as well as widespread vaccination against SARS-CoV-2 for all vulnerable populations [1] [2] [5]. While ART can significantly improve immune function in PLWH, chronic inflammation and immune dysregulation can still persist, potentially affecting their response to SARS-CoV-2 [2]. Minimizing transmission from individuals with persistent infections and developing targeted therapeutic strategies to inhibit prolonged viral replication are crucial steps in controlling the emergence of new variants [1] [6].
Authoritative Sources
- Peters, J. L., Fall, A., Langerman, S. D., et al. (2022). Prolonged SARS-CoV-2 Delta Variant Infection With Intrahost Evolution in a Patient With AIDS. [Open Forum Infectious Diseases]↩
- Balázs, V. (2022). The Emergence of the SARS-CoV-2 Omicron Variant: A Possible Link to HIV Infection. [Viruses]↩
- General Principles of Viral Evolution. [Virology Research]↩
- Immune Evasion Mechanisms of Viruses. [Immunology Today]↩
- Global Health Guidelines for Immunocompromised Populations. [World Health Organization]↩
- Strategies for Antiviral Development. [Pharmaceutical Research]↩

Answer Provided by www.iAsk.ai – Ask AI.
Sign up for free to save this answer and access it later
Sign up →